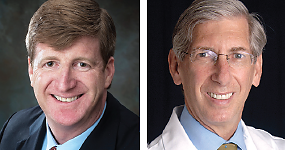
APA President Jeffrey Lieberman, M.D., is using the Psychiatric News Alert as a forum to reach APA...
The Truth About Psychiatry and Health Care Insurance
 |
A recent study by Bishop et al. in JAMA Psychiatry prompted a New York Times article (“Fewer Psychiatrists Seen Taking Health Insurance," December 11, 2013) and dialogue (“Invitation to a Dialogue: Hurdles to Mental Care,” January 4, 2014). This relatively limited study in a psychiatry specialty journal obviously touched a nerve and sparked a public debate in the media in which psychiatrists were not portrayed very favorably. From the article, one could conclude that psychiatrists do not accept insurance because it does not pay enough; they accepted patients only with “deep pockets,” and they were not willing to participate in provider networks.
Although there were elements of truth in the media coverage, the truth is more complicated, as is frequently the case. The truth of the matter begins with the fact that our country’s health care system is challenged by a shortage of mental health care providers, especially psychiatrists. Half the counties in the United States lack practicing psychiatrists. The inability to access care is further exacerbated by discriminatory, and often illegal, barriers to mental health and addiction services for patients imposed by insurance companies. Psychiatrists are routinely paid less for their services, even when they are using the same Evaluation/Management (E/M) codes, than other physicians and even though they typically spend significantly more time with patients. Patients with depression can see their primary care doctor or they can see a psychiatrist. However, primary care physicians, who are not as well trained in mental health care as psychiatrists, are paid more. In response to improvements to the CPT coding structure for psychiatry, some insurance companies reduced the rates they would agree to pay psychiatrists for E/M and psychotherapy. The Mental Health Parity and Addiction Equity Act prohibits this disparity, and APA has sued Anthem and WellPoint in Connecticut to end discriminatory reimbursement practices that lead to inadequate networks of psychiatrists.
Click here to read more.
Follow Dr. Lieberman on Twitter at @DrJlieberman. To do so, go to https://twitter.com/DrJlieberman, log in or register, and click on “Follow.”