Failure to Respond to Antipsychotics Early May Predict Long-Term Outcomes in Youth With Psychosis

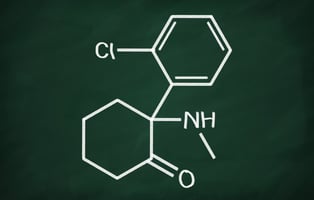
Adolescents with first-episode psychosis who do not respond to aripiprazole or quetiapine within four weeks appear unlikely to respond to the medications eight weeks later, reports a study in the Journal of the American Academy of Child and Adolescent Psychiatry.
“[Y]oung people with psychosis usually face years of psychiatric treatment, and pharmacotherapy is essential for recovery. Yet, antipsychotics should be administered with caution in adolescents due to an increased risk of side effects,” wrote Anne Katrine Pagsberg, M.D., Ph.D., of the University of Copenhagen, Denmark, and colleagues. “Being able to identify non-response early facilitates quicker decision-making to change treatment and, thus, diminishes the risk of prolonged exposure and adverse events associated with an ultimately ineffective medication.”
Pagsberg and colleagues analyzed data from the Tolerance and Effect of Antipsychotics in Children and Adolescents With Psychosis (TEA) study, a 12-week randomized, controlled trial in Denmark that compared the efficacy of aripiprazole to extended-release quetiapine in 113 adolescents (under age 18) diagnosed with first-episode psychosis. The researchers examined whether adolescents’ response to their assigned antipsychotic at two and four weeks could predict their response to the medications at 12 weeks. Non-response at Weeks 2 and 4 was defined as <20% decrease in the 30-item Positive and Negative Symptom Scale (PANSS-30) total score; non-response at the end of the trial was defined as <50% decrease in PANSS-30 at week 12. The analysis included 84 adolescents who adhered to their medication for all 12 weeks of the trial.
The researchers found that adolescents who did not respond to their assigned antipsychotic at Weeks 2 and 4 were about 80% and 90% likely, respectively, to not respond to the medication by the end of the trial. When adjusting for other variables, they found that non-response at Week 4 remained a statistically significant predictor of future non-response. They also examined other cutoff ranges and found that using a <30% symptom reduction at Week 4 offered the best predictive value for non-response at Week 12.
There were no significant differences between the two medications in terms of early and long-term response rates.
“In youth with first-episode psychosis showing early non-response to aripiprazole or quetiapine-extended-release, switching antipsychotic drug should be considered,” Pagsberg and colleagues concluded.
For related information, see the American Journal of Psychiatry article “A Population-Based Cohort Study Examining the Incidence and Impact of Psychotic Experiences From Childhood to Adulthood, and Prediction of Psychotic Disorder.”
(Image: iStock/Tassii)
Time to Vote in APA’s 2022 Election!
The voting period for APA’s 2022 election is now open. You can vote by using the emailed ballot you should have received by now or clicking on “Vote Today” on APA’s website. Take time to learn more about this year’s candidates by reading the Special Edition APA Election Newsletter and viewing the archived town halls in which candidates responded to key questions. The deadline to vote is January 31 at 11:59 p.m. ET. Your vote matters to the future of APA and psychiatry!