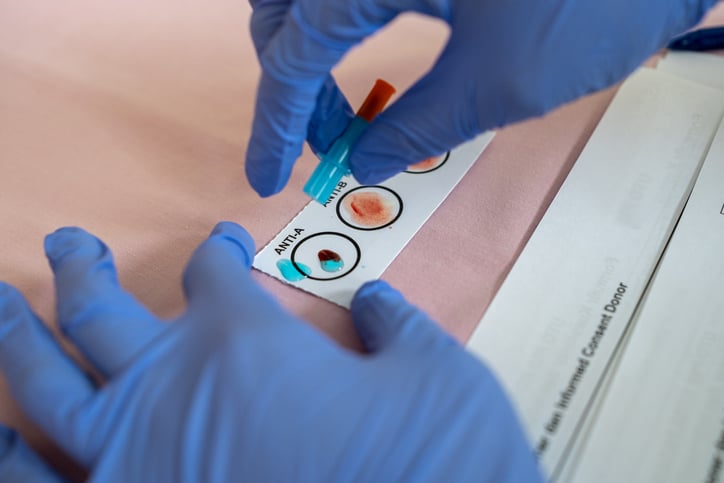
Levels of p-tau217, a validated Alzheimer's disease biomarker, can be accurately detected from blood...
Children with attention-deficit/hyperactivity disorder (ADHD) are more likely to receive negative pa...
Young people living in one of four states with flavoring bans for e-cigarettes were only half as lik...
As we head into a new year, many Americans are reporting anxiety about current events and/or future ...
Read the year’s top 10 most popular articles from Psychiatric News:
January The FDA approves the esketamine nasal spray Spravato as a monotherapy for adults with treatm...
Individuals between the ages of 25 and 64 who are on Medicaid had a higher rate of suicide in 2020 t...
Cannabis products that primarily contain cannabidiol (CBD) bring little relief to people with chroni...
Individuals largely misinterpret the instructions when completing the most commonly used depression ...