Researchers at the Mayo Clinic have identified a potential biomarker to identify which people would...
Study Finds Gabapentin May Be Effective in Treating Alcohol Dependence
 |
"This is an impressive and revealing study," Marc Galanter, M.D., a professor of psychiatry and director of the Division of Alcoholism and Drug Abuse at New York University, told Psychiatric News. "The authors, however, point out that approved medications are prescribed for only 9% of American alcoholics. Why is this? One reason is that for addiction, a chronic disease, clinicians are most likely to use medications with a demonstrated long-term impact, like buprenorphine for opioid dependence. The impact of gabapentin on alcoholism (like that of naltrexone) is a meaningful, but still limited step toward this goal."
On the other hand, as the researchers point out in their report, "Unlike other approved treatments for alcohol dependence that are prescribed by a small number of specialists, gabapentin may be more readily utilized by primary care physicians."
Information about how the outcome of alcoholism treatment may be determined by a person's genetics can be found in the Psychiatric News article "Genes May Determine Drugs' Alcohol-Treatment Success." Extensive information about alcohol dependence and medications to treat it can be found in the new American Psychiatric Publishing book, Clinical Manual of Addiction Psychopharmacology, Second Edition. Also see the report
"Gabapentin Combined With Naltrexone forthe Treatment of Alcohol Dependence" in the American Journal of Psychiatry.
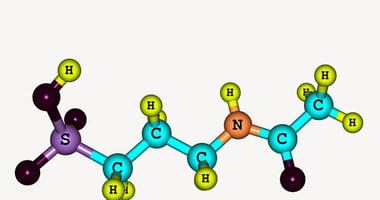
(Image: Alexey Lysenko/Shutterstock.com)