APA learned today that Medicare providers who file 1500 Health Insurance Claim Forms are having a...
Are Your 1500 Forms Being Rejected? Here’s Help!
APA has received reports that Medicare providers who file 1500 Health Insurance Claim Forms are having a large number of their claims returned due to a change in the reporting requirements that went into effect on October 1.
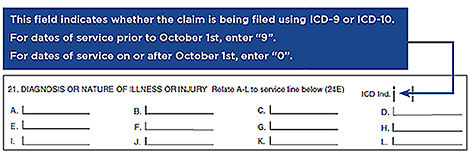
Medicare contractors are returning claims for correction or resubmission to mental health professionals who fail to indicate in line item 21 of the 1500 claim form whether ICD-9 or ICD-10 codes are used.
For services that were provided prior to October 1, ICD-9 codes should be used even if the claim is filed after that date; for services on or after October 1, 2015, ICD-10 codes should be used. ICD-9 codes are indicated by using a 9 in item #21; ICD-10 codes are noted with a 0.
Also, though there is some inconsistency among what payers are accepting, the general feedback that APA is receiving is that codes submitted in Item 21 should not contain a decimal point (for example, the code F43.10 should be submitted as F4310).
DSM-5 lists both the ICD-9 and the ICD-10 codes for each diagnosis. The ICD-9 codes are in black ink and the ICD-10 codes are to the right of them in gray ink.
For information about how to implement ICD-10 codes using DSM-5, see Using DSM-5 in the Transition to ICD-10.
We encourage you to provide us with feedback regarding any problems you have with the claims you file by sending an email to dsm5@psych.org. The more feedback we receive from you, our practitioners, the better we can communicate tips like the above to help ensure that your claims are accepted.
Medicare contractors are returning claims for correction or resubmission to mental health professionals who fail to indicate in line item 21 of the 1500 claim form whether ICD-9 or ICD-10 codes are used.
For services that were provided prior to October 1, ICD-9 codes should be used even if the claim is filed after that date; for services on or after October 1, 2015, ICD-10 codes should be used. ICD-9 codes are indicated by using a 9 in item #21; ICD-10 codes are noted with a 0.
Also, though there is some inconsistency among what payers are accepting, the general feedback that APA is receiving is that codes submitted in Item 21 should not contain a decimal point (for example, the code F43.10 should be submitted as F4310).
DSM-5 lists both the ICD-9 and the ICD-10 codes for each diagnosis. The ICD-9 codes are in black ink and the ICD-10 codes are to the right of them in gray ink.
For information about how to implement ICD-10 codes using DSM-5, see Using DSM-5 in the Transition to ICD-10.
We encourage you to provide us with feedback regarding any problems you have with the claims you file by sending an email to dsm5@psych.org. The more feedback we receive from you, our practitioners, the better we can communicate tips like the above to help ensure that your claims are accepted.