The mental health parity law appears to have been effective at eliminating quantitative treatment...
Federal Agency ‘Dead Set’ on Enforcing Parity, Seeks Psychiatrists’ Feedback on New Rules

The Employee Benefit Security Administration (EBSA) wants to hear from psychiatrists about recently proposed regulations to strengthen the 2008 Mental Health Parity and Addiction Equity Act (MHPAEA). The deadline to submit a formal comment on these proposed rules is Monday, October 2.
EBSA is part of the Department of Labor and is responsible for regulating 2.5 million employer-sponsored benefit plans providing health benefits to some 134 million people.
The new rules—proposed by the departments of Labor, Treasury, and Health and Human Services—are meant to close loopholes and add greater clarity to the law’s requirement. They were announced at an event at the White House on July 25 that brought together leaders of APA and other mental health and patient advocacy organizations.
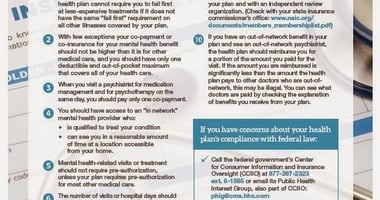
“The idea behind parity is that if an insurer is going to impose a financial condition or a treatment limitation on a beneficiaries’ receipt of promised benefit, those requirements and limitations cannot be more restrictive for people with mental illness or substance use disorders than they are for people with general medical conditions,” Tim Hauser, deputy assistant secretary for program operations at EBSA, told Psychiatric News.
But the reality, as too many patients and their psychiatrists have learned, hasn’t lived up to the vision. Hauser outlined ways in which the proposed parity rules would make the law clearer and remove loopholes that insurers and health plans have used to dodge the law’s requirements.
- Inclusion of a statement of purpose: The statement of purpose is designed, Hauser said, to remind everyone of the purpose of parity: When insurance companies are determining treatment limitations on a beneficiaries’ receipt of promised benefit, they can be no more restrictive than those for general medical conditions.
- Clearer definitions of terms and concepts: For example, the proposed rules clarify the meaning of “restrictive” limitations on mental and substance use disorder benefits.
- Mandating collection of data on outcomes: Under the proposed rules, insurers and health plans would be expected to continually collect data on outcomes related to “non-quantifiable treatment limitations”—those treatment limitations that are not financial in nature but include such things as requiring prior insurance authorization for a particular treatment.
- Requiring a written analysis comparing limitations: Congress approved a law two years ago saying that the departments of Labor, Health and Human Services, and Treasury can request a written analysis comparing mental and substance use disorder treatment limitations and those for medical and surgical treatment. “Our proposed rule defines how that analysis should work, what information insurers need to be providing us, and makes clear what the consequences are for noncompliance,” Hauser said.
Hauser urged APA members and others to respond with comments on the proposed regulations by the October 2 deadline. The agency is particularly seeking feedback from psychiatrists on reliable metrics that might be used to compare treatment limitations, he said.
“The problem with access to treatment is a serious one,” he said. “Fifteen years into the parity law, we should not be dealing with these issues. We are dead set on fixing it.”
For a full report, see the Psychiatric News article “Federal Agency Declares It Is ‘Dead Set’ on Enforcing Parity.”
(Image: iStock/Deagreez)
Don't miss out! To learn about newly posted articles in Psychiatric News, please sign up here.





-Jun-24-2025-06-18-45-4007-PM.jpg?height=200&name=shutterstock_143702539%20(1)-Jun-24-2025-06-18-45-4007-PM.jpg)